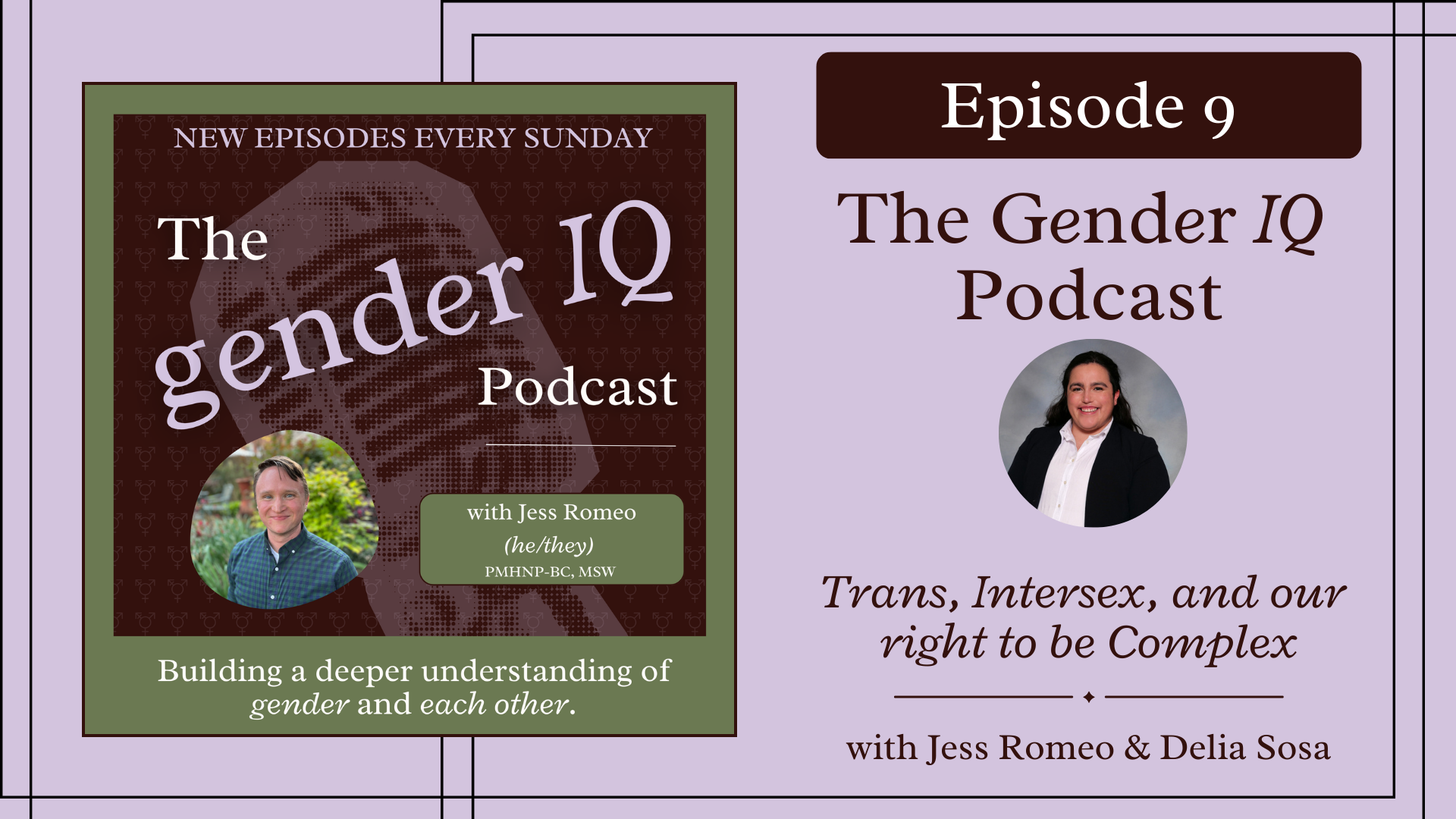
Episode 9: Trans, Intersex, and our Right to Be Complex
Queer people often have to trade truth for safety in healthcare - and we’re done playing by those rules.
Episode Overview:
In this episode, Jess and Delia Sosa explore what it means to be both trans and intersex in a system that rarely understands either. From navigating IVF to challenging medical norms, Delia shares how personal experience fuels their path toward justice-rooted care.

About the Guest
Delia Sosa (they/them) is a fourth-year medical student, a transgender and intersex advocate, and an LGBTQIA2+ educator. They are the Executive Director of the national Medical Student Pride Alliance and an executive board member of the Association of Native American Medical Students representing the Midwest. Delia has co-authored policy for the American Medical Association to strengthen protection for gender-affirming care across the United States and policy for their state medical association to prevent unnecessary surgeries on intersex youth and infants, improve insurance coverage for IVF, and protect DEI in medical schools.. Delia spends their free time creating educational resources and social media educational tools for healthcare providers and staff on how to care for LGBTQIA2+ patients.
There’s more than one way to come home to yourself.
In this episode, Delia Sosa shares their journey as a trans and intersex med student navigating identity, IVF, and a medical system that often fails the very communities they’re training to serve. It’s a conversation about complexity, courage, and building something better from the inside out.
👇 @enby.delia on Instagram 👇
Together, we discuss:
✨ What it’s like to discover you're intersex as an adult
✨ Navigating IVF, dysphoria, and the healthcare system as a trans couple
✨ Why intersex folks deserve care beyond being a footnote in trans health
✨ How professionalism in medicine can be a tool of white supremacy
✨ The long fight for bodily autonomy for all people
Explore our course on intersex care
If you're a clinician, educator, or advocate and this conversation inspired you to dive deeper into learning about intersex issues and paradigms for care, you can check out this lesson here »
This is a video from Jess' curriculum but made by Hans Lindahl - an intersex advocate and educator who runs the youtube channel @hihellohans. Hans further expands on the ways we think about gender, sex, and the systems that shape both.
Transcript
Delia Sosa: I mean, for me personally, like, it just doesn't feel complex. I'm like, okay, I'm trans and I'm intersex. Like, for someone who holds those identities, it feels very simple. The intersex community is a complex and beautiful community of people who have their own identity separate from the trans experience a different set of needs. So as we deconstruct the binary notion of gender as it exists, we also need to be deconstructing the binary notion of sex, not just for trans people, but for intersex people too.
Jess Romeo: Welcome to the Gender IQ Podcast. My name is Jess Romeo and I'm a psychiatric nurse practitioner, psychotherapist, and just an endlessly curious soul. I'm also a trans guy who specializes in working with queer and trans folks every single day in my private practice. I created this podcast because in a world that seems hell bent on using gender identity as a wedge to divide us, I wanted this to be a space for thoughtful, unfiltered, and nuanced conversations that help us connect with one another.
So wherever you are on your own journey, I'm glad to have you here.
Let's dive in.
Jess Romeo: Hey everyone, welcome back to the show. Today I'm talking with the incredible Delia Sosa. Delia is a fourth year medical student, a transgender and intersex advocate and an LGBTQIA2+ educator. They are the executive director of the National Medical Student Pride Alliance and an executive board member of the Association of Native American Medical Students representing the Midwest.
Delia has co-authored policy for the American Medical Association to strengthen protection for gender affirming care across the United States and policy for their state medical association to prevent unnecessary surgeries on intersex youth and infants, improve insurance coverage for IVF, and protect DEI and medical schools. Delia spends their free time creating educational resources and social media education tools for healthcare providers and staff on how to care for LGBTQIA2 plus patients. I'm so excited to have this conversation with Delia today, and I think you'll enjoy it too.
And just a note, if you think you're hearing a dog in the background for some of the podcast, that's not just you. Delia's dogs were hanging out, and you can hear them at some points during the podcast.
Let's get into it.
Jess Romeo: Well, so Delia, tell us a little bit about you. How would you describe yourself? Like, what's your little elevator pitch for who you are and what you do today?
Delia Sosa: Yeah, so just to kind of give you a very brief, like one sentence overview, I am a transgender and intersex medical student training to become a gender affirming provider.
I was born and raised in the Northeast, grew up there for most of my life in this like little Christian community where like gender and sex were not a thing. It was just like, "you are going to grow up and you're going to marry a Cishet man and you're going to make babies." And I was like, "do I want to do that? I don't know."
Jess Romeo: Mm-hmm. They had that where I'm from too.
Delia Sosa: I think that's pretty common across the US. So I lived there for the first 18 years of my life and then moved to Chicago for four years in undergrad. And that was really when I was able to be out for the first time. It was a very freeing experience being there and being in a city that is so affirming to so many people in the queer, trans and intersex communities.
Jess Romeo: Yeah.
Delia Sosa: Um, so that was kind of when I first realized that I was trans too. I sort of had like this gut feeling for a long time. I was like, "I don't think I'm a girl, but I don't think I'm a boy either. And I don't really know where I fit into this world." So I ended up coming out in 2021 as trans non-binary and then had top surgery in 2022. And the rest has just been kind of evolving from there.
Jess Romeo: As it does. Yeah, that's awesome. Well yeah, I'm always curious to hear people's stories in more in depth. like tell me about upbringing. I can imagine it, but what do you remember learning about gender or being taught about gender from an early age?
Delia Sosa: Oh, I love this question. There was so little that was taught about gender from the time I was a kid. Like I remember being on the porch of my mom's house when I was like, I don't know, seven or eight. And I was like, what's the difference between gender and sex? Like I was asking my parents and I think, I don't remember if it was my mom or my dad that said this, but one of them was like, they mean the same thing. Like gender and sex are exactly the same. And I don't fault them for this because I think that was the understanding that they had at the time. But it wasn't till like towards the end of high school that I actually learned what it meant to be trans. That was when I discovered Skylar Baylor's story. Because I was also a swimmer. So when I heard about Skylar's story, I was like, "whoa, yeah wow cool yeah."
Jess: Because wait - about how because - I'm in like mid 30s. Are you younger than me to a significant degree or we have the same?
Delia Sosa: I'm late 20s, so a little bit younger. Yeah. Yeah.
Jess Romeo: Okay, so yeah, a little bit of a half generation difference. So we're talking about 2000s or to 2010s that this is happening.
Delia Sosa: Yeah, yeah, like 2010 to 2015, I would say was around - around when this is happening. So yeah, towards the end of high school is when I heard about Skyler's story and one of my best friends from high school came out as trans around the same time.
Jess Romeo: Got it. Okay.
Delia Sosa: At the time, I think I sort of had an inkling like "something feels like this fits," but I was not in a place where I could explore it. I was in an all girls Catholic high school where like everyone was very like, "yay women." And it's like, "what about other people?" So, you know, my parents growing up were very accepting of people in the LGBTQ plus community, but I don't think they fully understood all the nuances of being part of that community and the nuances of each of those identities. So it really took a lot self-exploration and self-education to figure that out. And it wasn't until I got to college that I was able to do that and had the resources to do that.
Jess Romeo: That is so many people's stories. Even if you grow up in a fairly accepting place, I think there's just something, there's something about that stage of development and that going away, being in a new space and not being tied to those roots that can make a big difference. Okay, so that's actually helpful in knowing our age difference, because we're about eight years apart. So what I remember about gender in the 90s was, on our faces, we said the, do you remember, do you get the reference of like the Mia Hamm, Michael Jordan commercial where it was just like anything you can do, I can do better.
Delia Sosa: No, I wish I did.
Jess Romeo: It was very like - out of the front of our mouths. We said, "women can do anything that men can do." And then from the back it was, "but that's all that exists. And women really can't do everything that men can do. And actually we're going to be very anti LGBTQ the entire time we're saying this.
But okay, you get to college. And then, so coming out as trans, and then I know you're like trans and intersex. And a lot of people think that they struggle with those identities too. How did you become aware of an intersex variation or come to identify that way?
Delia Sosa: Yeah, so it was an interesting experience because I had been having like chronic pelvic pain for several years. Like it started, I want to say when I was like 21 or so. And by the time I got to be 26, it was still happening. It was not a pleasant experience.
So I started seeing a new gynecologist and she was incredible. Very affirming, very accepting and open and willing to learn. Like she was able to acknowledge like what she didn't know. And we were talking about the possibility of me having endometriosis, because that's what it sounded like based on the pain that I was having and the other symptoms that went with it. So she said - we had tried oral birth control pills to manage it. And I found out I can't take those because my blood pressure gets way too high.
Jess Romeo: Oh no. Okay, yeah. Mm-hmm. Happens to some people.
Delia Sosa: Mm hmm. Exactly. So she was like, "okay, well, your other options are to try an injection or to do surgery and see if you actually do have endometriosis." And I was like, I don't want to go through the injections, I don't want to keep trying medication and just see if it works or not, like I just want to know definitively if I have it. So she said that we could definitely do the surgery, but she wanted to do an ultrasound before the surgery to just make sure there was nothing else that she was missing before we went in. And on the ultrasound, that was when they found out that I have an intersex variation. Yeah.
Jess Romeo (08:45)
Yeah, fair. Wow, yeah, that would make sense in the steps needed before the surgery and also why they wouldn't discover that beforehand.
Delia Sosa: Yeah, exactly. Like, I had had normal periods, I had never had anything besides facial hair that made me think that I could have an intersex variation, and then it just was found on an ultrasound and I like, "wow, okay, cool, this is part of me I didn't know about."
Jess Romeo: Why would you? Yeah. And I love how, too - so there's something that happens with, I think, any person who's queer, but especially with trans folks and with intersex folks, where people get really curious about the details of things very quickly. And I really appreciate how you even set the boundary in how you described, like, "they found an intersex variation."
Delia Sosa: Thank you.
Jess Romeo: Because that's all people need to know. Like, people do not need to know what the details are. And in fact, that is often kind of a lurid thing for people. Like there are a lot of different intersex variations. You can look it up online and find out what this means, but what does it mean to you? What did that shift for you in realizing that was the case?
Delia Sosa: It was actually very affirming for me. I had started developing facial hair a couple years before I found out I had an intersex variation and my primary care doctor was trying to figure out like, okay, is there like a tumor that we need to be worried about? Like, is there something really serious that we have to be worried about?
Jess Romeo: Yeah.
Delia Sosa: I do a lot of, like, education online and people had started noticing that I was growing a beard effectively and I was getting a lot of comments about it like, "why do you have boobs and a beard?" I'm like, "well, first of all, I don't have boobs anymore. I cut them off. Second of all, it is possible to have both and that's a valid part of being intersex for people with some intersex variations." So to know that like my body wasn't just growing a beard for no reason was very validating. It was like, okay, this is just part of who I am. It's not something that's inherently wrong with me. It's just me.
Jess Romeo: Yeah. Me six months on T would have been very jealous of your facial hair. There was one time I had a patient who'd started T and within six months he like full beard and I just couldn't hide the jealousy. I was like, "come on man, like that's just not fair. You're just, you're just like, flaunting this out here." But it was nice because we were able to just connect like two people.
Delia Sosa: I love that. That's so beautiful.
Jess Romeo: Yeah. So I could appreciate how it would feel really affirming to learn that. Do you actually know the story of Pauli Murray?
Delia Sosa: No, I don't.
Jess Romeo: Pauli Murray - I'll use, I'll probably go back and forth between she and they pronouns, but they were a civil rights activist back in the thirties and forties and were part of, they were part of the team that brought the Brown v Board decision to the Supreme court, worked with Thurgood Marshall. And in the forties, they were involved in a lot of bus boycotts that were just, they were prior to 1955 Montgomery. So they aren't taught as part of civil rights. We don't know them as well.
But they were a law student and an attorney, but they suspected that something was off regarding gender for them. I don't know how they would identify today, right? It's one of these things where we can't apply our current concepts of transness onto a historical figure, but they were writing to doctors asking for imaging, essentially, saying, "I suspect I may have internal masculine parts -
Delia Sosa: Wow.
Jess Romeo: "- and I feel like I would like to be able to have treatment to live into who I actually am. It's really a fascinating story. There's a documentary out there, but just that feeling like, "I just see if what I feel has some evidence for it? Please, like someone just show me that it's real."
Delia Sosa: Wow. Yeah, wow. Honestly hearing that story is also really affirming in a lot of ways. Because I think for a lot of intersex folks or people who suspect that they may have an intersex variation, there's kind of this lingering question of like, "what am I missing? And how can I get answers to the questions that I want to know?" Like I get questions pretty often from people who suspect they have an intersex variation of like, how can I find out if I do have one? And there's not really a clear-cut answer because there's so many intersex variations out there that the answer could be in looking at like all the chromosomes in your body or looking at the chromosomal distribution in different parts of the body. It can have to do with the hormone levels in your blood or what anatomy you have. So there's no like one clear-cut test to say like, yes, you are intersex. And that's a really difficult thing to grasp for some people and a difficult thing to accept, especially if you have this gut feeling like something is different.
Jess Romeo: Right. Yeah. And I know that I'll link for anybody who's listening, I'll link some things in the show notes around - there's a good Scientific American article reviewing a lot of various intersex variations. Since you are the med student here and an expert in this content area, kind of run us through the different - just sex differentiation, kind of a basic level and where intersex variations can show up for people at what levels.
Delia Sosa: Yeah. Yeah, so I kind of like to think of sex as being five different baskets and everyone has some combination of eggs in each basket, but each person's combination looks a little bit different. So the five different components are genes and chromosomes -
genes being like the specific sequences of DNA that code for certain things in the body and chromosomes being the way that those genes are organized. Epigenetics, which is how genes are regulated in the body. And there's there can be temporary and permanent changes in every person's epigenetics will look a little bit different and can change over time. There's internal anatomy, which is typically uterus, ovaries, testes, adrenal glands, that's a really important one that is not necessarily a reproductive organ, but does play a role in some intersex variations. There's external anatomy, which would be like vulva, penis, clitoris, like all of those different components, or some combination of the above. And then there are hormone levels. So hormones are interesting because we all have some combination of these same hormones, but the way that our body processes and uses those hormones is different depending on how much of each hormone is present in the bloodstream, depending on how many hormone receptors are present in the body, depending on where those hormone receptors are located, and depending on whether those hormone receptors are functional or not. So in any one of those five buckets or in multiple of those buckets, there's an opportunity for variations to pop up that we would call intersex variations.
Jess Romeo: Mm-hmm. That's a really good way of describing it. I - do you know of Hans Lindahl, the YouTuber?
Delia Sosa: I don't, no.
Jess Romeo: So I created a curriculum on trans affirming care a couple years ago when I started this work and I was like I want to I want to prioritize lived experience and lived expertise and I know we need to talk about intersex topics. That is not my lived experience. And so Hans came in and did a really amazing lecture that was pre-recorded for the course, but I was obsessed with Hans' YouTube content because Hans will talk about hormones as juice. Like there's still the split that Hans talks about, but that yeah, sometimes the receptors don't actually work or this hormone will actually be expressed vastly differently in my body versus yours versus someone else's.
Delia Sosa: Yeah, exactly. The hormone piece is so fascinating. And I think there's a common assumption that like, men have testosterone and women have estrogen and it's split down the middle like that. But that's not actually the case. We all have testosterone and we all have estrogen and we all have progesterone. It's just how much of it is in each of our bodies and how is it being used by our bodies?
Jess Romeo: Right. Yeah. So the five different baskets, as you're doing education on this, where do you find people either get the most captivated? Like, "oh my god, I never thought about it this way" or get the most lost. And that might be the same place.
Delia Sosa: Yeah, it kind of is the same place typically. So I typically start off any lecture that I give on this topic by explaining like the different ways that we determine sex, either in utero or when a baby is born. And I think that I always tend to see people's eyes bug out a little bit and then they're like, wait a second, everything that I've been taught is different.
So just to kind of give a brief overview of what that looks like, there are a few different ways that we can test for sex. So we can look at an ultrasound. It's literally just like, is there a little baby phallus or is there no baby phallus?
Jess Romeo: Yeah, just external anatomy only. That's all that tells you.
Delia Sosa: Mm-hmm, exactly. And then you can also test the birthing parent's blood to see if there is the presence of a Y chromosome because theoretically the birthing parent should not have any Y chromosomes. Sometimes they do, so that's not an entirely accurate test, but theoretically they shouldn't. So if there's a Y chromosome, it's a male, or at least we expect it's a male.
Jess Romeo: Yeah.
Delia Sosa: Another way is to actually sample the amniotic fluid within the uterus. There's risks that come with that. people who do that testing have to talk to patients about the risk versus the benefits of doing that. But you can do a chromosomal analysis with the amniotic fluid. Or you can wait till the baby is born and see, do they have a phallus or do they not have a phallus?
Each of these ways of testing for sex doesn't include the intersex experience because
Jess Romeo: Exactly, yeah none of them do.
Delia Sosa: Like let's say you have someone with complete androgen sensitivity syndrome, for example, someone with CAIS would have XY chromosomes, but would not have a phallus on ultrasound. So if - those two, if there was a discrepancy between those two, like everyone's minds would be blown. They're like, what is going on with this baby?
Jess Romeo: Mm-hmm. Yeah, they'd be going back and checking the chromosomal analysis, like something there's a mismatch here, but the, you know, it's a baby that would phenotypically look female. External anatomy looks female. We have XY chromosomes and that's an intersex variation. You wouldn't know that there was a discrepancy unless you had done a chromosomal analysis.
Delia Sosa: Mm-hmm. Yeah, exactly. But I think that part kind of blows people's minds. They're like, "wait a second, we can't just tell sex by looking at an ultrasound?" And it's like, "not always, no."
Jess Romeo: Yeah. No, it drove me nuts. Like I'm a new parent. Like kid is about eight months old now. And God, every time we went to the ultrasound, they're like, "are you finding out gender?" We're not finding it. Cause we decide, I know every single time when they said gender and I wanted to - I didn't feel like causing a stir each time we went to the OB's office. Also, it was not my body. I was not the birthing parent. So I was like, "I am here to support. I'm not here to like cause a scene."
But every time I just wanted to say, "oh, it's not even sex." It's like just, you're talking about genitals. You're not talking about gender, you're talking about genitals. And that's why I think they don't say it. Because gender is such a more pleasant term than to say, what do you want to know about your baby's body parts? Like, get real, that's what we're asking.
Delia Sosa: Literally. Exactly. Well, there's also the assumption that every person who has a child is going to raise that child under the societal norms that go along with those genitals. Like the assumption that if you have a penis or if your child has a penis that you're going to raise the child to be a boy or that if the child has a vagina that you're going to raise the child to be a girl. And it's like, well, that's not the case for everybody.
Jess Romeo: Right. Yeah.
Delia Sosa: You know, some people are going to raise their children in a more gender neutral way. Some people are going to let their kids figure out who they are before starting to assign any kind of gender to them, you know?
Jess Romeo: Yeah. Yeah. And that can look so many different ways. I remember talking to a friend about this recently because we're not doing the they them pronoun thing for our kid. Again, like I think we have to at our own nervous system levels, like having to explain that to parents and family who are all from the South was just like, no, we're, we understand how we want to raise a kid within these gendered boxes and how to navigate that.
Delia Sosa: Yeah.
Jess Romeo: But I wish there were a pronoun in the English language that was just for children from like zero to five. Like just a child pronoun that you didn't have to choose gender. It's just, this is what it is.
Delia Sosa: Yeah, I do too. Mm-hmm. Yeah, I do too. My husband and I are working on family planning and IVF stuff right now and we've had a lot of these conversations like "how do we want to refer to our kid?" Because we also have to think about safety. Like, we live in a state that is not safe for trans people so we have to consider not just our safety but the safety of our kid too. Like, do we want to risk their safety for the sake of raising them in a more gender neutral way. I don't know.
Jess Romeo: Yeah. And I think these are, what's important for people to know is that these are calculations that any queer person is always kind of having to make and our expression of ourselves is sometimes going to be through that lens of safety.
Like it just is. You can only do what's safe for you and your environment. I could only express what was safe enough and what I had language for in my environment growing up. And so as much as we're seeing people live into themselves more authentically and we're seeing trans folks be more visible than ever before, it also is through a very dark lens right now too. And there's a lot of lack of safety too.
Delia Sosa: There is. mean, we just witnessed the death of Sam Nordquist recently. Trans people are risking our safety every single day to be who we are. And sometimes even when we take the best possible precautions to keep ourselves and our community safe, it's not enough because of the world that we live in.
Jess Romeo: Yeah. Yeah. Unfortunately, so.
Delia Sosa: But we do the best that we can.
Jess Romeo: Yeah, we do. How's the IVF journey going for y'all?
Delia Sosa: *Laughs*
Terrifying. We just did the egg retrieval a couple weeks ago. So we're glad that that part of that process is done. We decided to use my husband's eggs and my uterus for a variety of reasons. So I'm really happy for my husband that that part of the journey is over because that was incredibly difficult for him to go through. So I'm very happy that that part's over and that my husband can have that part of his life back.
Jess Romeo: I'm so glad too. I know a couple of folks who've gone through egg retrevials recently it is possible to stay on T while doing that. I don't know if that's what he was able to do or not. And even with the addition of the other hormones you have to take, can still be incredibly dysphoria inducing. But a lot of people didn't know that that's something they could do.
Delia Sosa: Mm-hmm. Getting into my med student brain for a second here, but part of the problem is that we just don't have enough data and we don't have enough research on long-term outcomes of fertility preservation for people who have stayed on T.
Jess Romeo: Yeah. Yeah.
Delia Sosa: Which makes it really difficult because it is a very dysphoric process and there are ways to manage dysphoria during the egg retrieval process. Like there's a medication that you can use called letrosol that kind of helps kind of dampen some of the dysphoria, but it doesn't make it go away completely, especially because every person's experience with their dysphoria is going to be a little bit different. So we really just, if anyone's out there listening who is really interested in IVF and cryopreservation, we need more data on this, especially for trans people who have been on T.
Jess Romeo: Yeah. Yeah, we absolutely do.
Well, so med school, like how did you always know you were going to be a doctor? Always know OBGYN was going to be your thing. How did you get to career part?
Delia Sosa: Yeah, so I always knew I wanted to be a doctor from the time I was like a little, little kid. I was telling people like, I'm going to be a pediatrician. Don't want to be a pediatrician now, but - kids are cute, I just don't want to - I don't want to be a pediatrician. The OBGYN part came a little bit later. My mom was actually a labor and delivery nurse, so I
Jess Romeo: Wow.
Delia Sosa: Yeah, yeah. I got exposed to obstetrics and gynecology from like a kind of a young age, which sounds a little bit strange. But for me, it was actually really interesting. Like, I feel like I got to learn a lot from my mom and I got to see part of the medical world that I wouldn't have gotten to see otherwise.
And the more time that I have spent in med school, the more I've kind of realized like, I want to work at the intersection of reproductive rights and reproductive health and LGBTQ health, specifically like for trans and intersex people who may have previously had a not so affirming experience. I think there's a lot of great work that has been done in OBGYN and there's still a lot more work to do.
And I couldn't really see myself going through all of med school and all of residency, only to not be part of that. So that's kind of how I ended up there. Still trying to decide if I want to do like general OBGYN or if I want to do reproductive endocrinology and infertility, which would basically be the IVF process.
Jess Romeo: Yeah, that's great. You would be able to help with some of that research that is desperately needed. Yeah, that would be huge. I mean, it makes sense. Like this is, I think we each move into the places in the field, in the movement, in the resistance, the revolution, whatever you, whatever you want to call it, where we can make the most impact. Like for me being a clinician and then a psychiatric provider, that's where I feel like is the best fit -
Delia Sosa: Exactly. Yeah.
Jess Romeo: - for me and god is this just perfect for you. One thing that I've heard from some folks is just the importance of talking about the fact that some intersex folks that I'm aware of have had some of the worst healthcare experiences actually within trans affirming healthcare spaces. And I wonder if that's something that you could speak to or have any thoughts or opinions about.
Delia Sosa: Yeah. Yeah. Yeah, I will say this is not an experience that I have had personally. I would encourage folks who are listening to seek out stories from intersex people who have had not so good experiences in trans health spaces. I think from what I understand and what I have heard, there are some assumptions that if you are in a trans health space that it is automatically inclusive of intersex people because there's sort of that notion that like, it's the same medications and it's the same procedures and trans and intersex people have a lot of overlap in terms of their marginalization and their medical needs. So why wouldn't it be the same thing? But there's actually a lot of - there's a lot of overlap between the two, but there's a lot of distinction between the two as well. There's different kinds of trauma that trans and intersex people have experienced in medicine. There is a lack of assent in a lot of the care that's provided to intersex people. I hate even calling it care because it's not truly care, it's like providing medication and surgery without that person's knowledge or consent.
Jess Romeo: Right, it's enforcement of normative sex and gender before someone can even consent or assent or be aware that that process is even happening.
Delia Sosa: Yes. Exactly, that is a fantastic way of phrasing it. And I think, you know, the other piece of it too is that with a lot of intersex variations, there are lifelong consequences or lifelong risks from having some of those intersex variations.
Like just to give you an example PCOS, which is an intersex variation but not everyone with PCOS identifies as intersex. One of the big risks of having PCOS is type 2 diabetes, which is a lifelong chronic illness that has plenty of other implications in and of itself. And if you are someone who is seeking access to care for your PCOS and a provider doesn't know that type 2 diabetes as a risk factor, it is incredibly difficult to trust that the care that you're getting is adequate. And that happens with a lot of different intersex variations, because there's not enough training on what each of these variations means, and what the long term implications of that are. And there's not a lot of research on it either.
So there's kind of like a social and environmental aspect to not feeling safe in trans health spaces, but then there's also like a medical aspect to it as well.
Jess Romeo: Yeah. Yeah, that's interesting. It's like being so many people, the LGBTQIA plus alphabet, the more we use it, and I have no issues with the alphabet itself, but I think it does perpetuate this idea that we're all in the same bucket and we have the same experiences. And this is how Cishet people have sort of looked upon us queers for many millennia, just saying like "something's up with those weirdos over there" and lumping sex, gender, sexual orientation like all together in the same bucket as if they all go together. And that's still going to be an easy fallacy for us to make like, okay, intersex folks, must have the same experiences as trans folks. They can go to the same clinics, but the experiences are wildly different.
But does it take really expert specialized care? Like I'm not an endocrinologist, I'm not even a primary care provider, but I can't imagine that the intersex variations themselves and then their medical sequelae that you have to monitor long-term, I can't imagine that that's wildly complex.
Delia Sosa: Usually it's not. Of course, there are exceptions to that. And it gets a little bit more complicated if you have more than one intersex variation as well. But it's really not as complicated as it sounds. It's just that we don't have a lot of training on it. Like I think at my med school, we had one lecture on intersex variations. And that was it. And we didn't even talk about like the long term implications of those. Are you familiar at all with Alicia Rothweigel?
Jess Romeo: No, I'm not.
Delia Sosa: Okay, so they are this incredible intersex activist currently based in Austin. And she actually has done a lot of work with a group of clinics in Texas called the Kind Clinic on -
Jess Romeo (34:02)
That I have heard of.
Delia Sosa: Yeah. And they basically - like Alicia and the Kind Clinic work together to make sure that intersex patients across the state of Texas would have access to like safe and intersex affirming care. And it's really incredible. They did this like whole big analysis and it's, yeah.
Jess Romeo: That's awesome, I'm gonna look into that for sure.
Delia Sosa: Yeah, I would. If you have a chance to talk to Alicia at all about it, it's absolutely incredible. The work that she did and the work that Kind Clinic did.
Jess Romeo: Yeah, and it's interesting - I think there's this way in which, and I'll own up to this for myself in thinking about educating around trans affirming care. To me, including intersex topics was both an interest in and of itself, but to be honest, it was more of a means to the end of a thesis that not only is gender not binary, but neither is sex.
It is bimodal and here are all of these things. And I was thankfully kind of called in to be like, Jess, this is also an entire community of people that is important to represent within this. But I think there's a lot of learning that I had to do along that process. Do you think there is value in holding some space for that without using intersex as a way of making the argument?
Delia Sosa: Yeah, absolutely there is. You know, I think intersex folks often hold space for trans folks, and trans folks can absolutely return that as well. I have seen a lot of that similar argument of like, "gender's not binary, but neither sex." But I think it's also, you know, as we're making that argument, it's also worth saying like, the intersex community is a complex and beautiful community of people who have their own distinct identity separate from the trans experience and who have a different set of needs as a community that are not being met by society currently. So as we deconstruct the binary notion of gender as it exists, we also need to be deconstructing the binary notion of sex, not just for trans people, but for intersex people too.
Jess Romeo: Yes. Well said. Really well said.
Delia Sosa: Thank you.
Jess Romeo: Well, talk to me about what some of those different needs are. This is where I figured we would talk about - what are the non-consensual surgeries? What are we fighting against here for children?
Delia Sosa: Yeah, so for those who may not be as familiar, there's a lot of trauma which has led to mistrust and distrust within the intersex community around medical spaces and around healthcare. And a lot of this stems from surgeries that are being performed on intersex youth and infants without their knowledge or their ascent.
This is a very complicated issue because there are arguments about like, well, you know, the parents have the right to decide what to do for their children. But in a lot of cases, the parents are also not being given adequate information to make an informed decision for their children. Historically, a lot of parents have just been told like, "there's something wrong with your child. We have to fix it" but not given a full explanation of what is actually going on and what they're going to do to fix it, quote unquote.
Jess Romeo: And what's usually the case that - we're talking about like external anatomy? Is that the only situation that you're talking about right now?
Delia Sosa: And also internal anatomy too. So there have been intersex youth and infants who have had their ovaries or testes, like internal testes removed because of a supposed cancer risk that I actually don't know that we have great data on. I need to look into that and do little bit of my own research on that too. But I - to the best of my knowledge, we don't have a lot of good data showing that there is an increased risk of cancer for people who were born with internal testes, or ovaries if they have a penis. So that's one of them. There's changes to external genitalia, which I will say that there are some intersex variations where medically that is necessary, but those are few and far between. It's -
Jess Romeo: Like if urination is impacted, things like that. Yeah.
Delia Sosa: Correct, yes. Urination, defecation. But other than that, I personally am of the belief that it should be up to each individual person to make that decision for themselves, unless it is medically necessary when they are young. So those are the kind of things that I am aware of. I'm sure there are other surgeries that I am not aware of and I need to do my own learning there too.
Jess Romeo: You're still a med student, like we're not expecting you to know everything here.
Delia Sosa: Yeah, I'm also a med student who's not going into pediatrics or pediatric urology, so will likely not learn a lot about these in depth unless I do my own digging, like on my own time.
Jess Romeo: Hmm. Yeah. That's fair. Yeah, who's the Delia of pediatric urology that I could talk to?
Delia Sosa: I'm not sure there is one.
Jess Romeo: Yeah, no, probably not.
Delia Sosa: There's a little bit of a tenuous relationship between the intersex community and pediatric urology.
Jess Romeo: I can imagine and like, I know that some people, it's so hard within the academy, because there are these providers who absolutely with full conviction believe that they are doing their best for their patients. And you have what's been described to me by other intersex activists who are doing education in healthcare spaces is that many providers who would be, know, pediatric urologists, they'd be doing these surgeries where it's essentially genital mutilation. Like that's what intersex communities would describe it - many intersex communities would describe it. But these urologists are being told that, well, the patients want this. Like they're going to want this. We need to fix it. Because if it's not normal, then they're not going to be OK. Like outcomes are better if you make this change when they're an infant.
And that data very clearly is not the case. Like that data doesn't exist. In fact, we have a lot of data to the opposite of that. But I think there's a lot of shame and self-reflection that a provider would need to sit with in order to think, oh my god, how many of these have I done? Thinking that I was doing the right thing. That's a lot for an individual to face. And so I think it can be hard. I think where we learn is with new generations
of providers who are in these rooms and in these situations.
Delia Sosa: Absolutely. I think from a statistical perspective, there's also some bias in the data that a lot of pediatric urologists have access to because - and I'm just using an anecdote from a study that I was presented at a conference. So there was a pediatric urologist that I listened to - a lecture that she gave on intersex variations and surgeries performed on intersex infants. And she was showing the results of her study, which showed something like 90 something percent, I think, of the patients that she continued to see were satisfied with the results of their surgery. But there was a very clear bias in that this was only coming from the patients who continued to see this provider.
Jess Romeo: Right.
Delia Sosa: Like what happened to the patients who didn't continue seeing the provider? And we don't know what the attrition rate was. And I think there's a lot of unintentional bias in the data that we have in the pediatric urology world and just in the medical world more broadly. think historically.
Jess Romeo: Uh-huh, yeah, what was the attrition rate here?
Delia Sosa: Intersex experiences have not been an important part of the story and there's a lot more room for growth and for learning as far as incorporating the actual lived experiences of intersex people who have been subjected to surgeries or other treatments without their knowledge
Jess Romeo: I mean, how do you see the role of healthcare providers in starting to change this? I'm talking for nurse practitioners, for doctors of all different specialties. Like, what do you think we should be tasked with to change this?
Delia Sosa: That's a fantastic question. Yeah. The first and foremost thing I would say is to really listen to what your patients have to say and be open to not necessarily criticism, but open to hearing about the experiences that they have had and the consequences of those experiences.
I think, at least in medicine, intersex voices have consistently been left out. So if we as providers are able to listen to our patients and not just find ways to create a sense of safety and comfort in that clinical encounter, but to find ways to use the feedback and the experiences that we hear to make the system better for other people who have an intersex lived experience, that's one of the best things that each of us individually can do.
On a broader scale, there's a lot of room for growth around writing policy for major medical and other healthcare, like, professional associations. There's room for educating other people on what it means to be intersex, not about sharing other people's lived experiences with people who may not be the best person to tell about those experiences or who may not have the right to know about those lived experiences, but to teach other people about the fact that intersex people exist and what it actually means to be intersex. And I think finally there's an opportunity to advocate against harmful legislation like gender affirming care bans that specifically have carve outs allowing surgeries on intersex youth and infants, testifying against those carve-outs and making sure that people know that gender-affirming care bans don't just affect trans people, but they also affect intersex people.
Jess Romeo: There's nothing more telling to me about the ideology behind these policies than when those carve-outs are specifically there in those bills. That's what we're doing. It's very straightforwardly "you will fit into the norm or you don't exist to me. I don't care what happens to you." It's really interesting.
I've been trying to think about this in different ways. Because the fields like healthcare fields, medicine, science, like in many ways tries to be as objective as it can. And I think in some fields that's easier than others. And there is some good objectivity. You know, I'm not a theoretical physicist, but I think they can have some objectivity. But when it comes to people and especially people's behavior, their way of engaging with the world.
We can't deny that it's like we exist in a cultural stream almost. That's the image that's been coming to me, especially when we're talking about that presentation from the urologist - things that go along the stream, like go with the stream of what the culture believes, just are not really questioned. Like we don't ask the extra question about, "does this make sense?" Because it's just going right along with how everybody else is thinking. Like, and I know more about the history of trans healthcare. Right?
So when that's back in the 70s, 80s, 90s, and almost till today, but it used to be much worse that if you needed to pursue a surgery, not only did you have to tell a very specific story, but you had to pretend that you were going to be straight. Like you had to say, "yes, I want to have a heterosexual partner. I want to be normal." And that the fact that we just don't question these things if we're going with the stream, but god forbid people want to live into their authenticity and feel liberated - the second that goes against a stream - all of a sudden, that's where gatekeeping comes in.
Delia Sosa: Yeah, exactly. And in - in medicine, especially there is, there is this notion of professionalism. Like, this is something that we're taught in medical school is the concept of professionalism.
And while I think there is something to be said about, you know, responding to emails in a timely fashion and being respectful towards every member of the team and showing up on time and all of those things, there's also a lot of white supremacist and patriarchal underpinnings to professionalism as it currently stands. Yep.
Jess Romeo: Yep. Yeah, you don't see the faces we're making, but we are making faces. I'm just like, "mm-hmm, I get it."
Delia Sosa: Yes, yes. It's like the notion that your hair can't look a certain way, or, you know, men have to wear a tie and a button down shirt under their white coat and women have to wear X, Y, and Z things, but there's no dress code for non-binary people.
Jess Romeo: Do you get to do whatever you want then?
Delia Sosa: That would be nice, but no. I think when we had the presentation on dress code at the beginning of my first year of med school. I asked a question of that, I was like, "what did non-binary people do? And they were like, I don't know, just pick one." I was like, "okay, sure, I guess."
But part of the idea of professionalism also plays into what we are and are not allowed to say. You know, if you're - you're going to be sharing information medically, it has to be accurate and it can't be hateful or directing discrimination towards a certain group of people. Because the reality is that everyone deserves access to health care. It's a basic human right. But I think there's kind of a discomfort when we're having difficult conversations specifically around marginalized communities. It's not just about, "I going to say the right thing?" It's also about, "will I still be able to care for my patients properly if I say something that goes against a societal norm that has contributed to medicine in some way?" Like, "will I be penalized? And not only will I be penalized, but will my patients be penalized?"
Jess Romeo: It's a really hard thing to hold. It's really, really difficult. I can't imagine, like - what kind of conversations are you having with other students or with professors? How is that conversation happening in med school right now?
Delia Sosa: Yeah, so there's a lot of conversations, particularly in my school right now, around gender affirming care. I talk about intersex care a lot, but it's not a larger conversation that we're having at my school. But there's a lot of conversations about gender affirming care and like the implications of what we say to our patients. You know, I think there's a lot of concern across the country right now about gender affirming care and access to it, not just for youth, but for adults as well. And we're having a lot of difficult conversations right now trying to figure out are our patients going to be able to continue to access this care. Who is going to challenge this care? Who could ultimately take it away from our patients and cause some pretty significant harm for our transgender and gender-expansive patients? We're trying to figure out how to fight against harmful legislation and harmful policy in a way that doesn't put our patients in harm's way and doesn't jeopardize our patient safety or their access to health care.
And these are really difficult conversations that we're having pretty much every day with each other, with our mentors, to a certain degree with the school as a whole, but that - that kind of depends on what the conversation is. Really, the biggest concern is just for our patient's safety at this point.
Jess Romeo: Understandable. It's hard to even know where to go from that. It's just, it's just so dark right now. But I think that it really does underscore one of the biggest differences that was there in the seventies with just LGBTQ plus rights movement is that when it really fractioned off to be more about gay and lesbian folks as opposed to trans folks and trans folks kind of got left behind, it's - a lot of trans folks' fight at that time was much more aligned with those who were fighting for Roe v. Wade. It was a lot more about bodily autonomy and being able to make decisions about your own body. And that I think is where all of these communities are very aligned today. Like you said, many differences, but I think that intersex folks, trans folks, and cis women all have a huge stake in what's coming next. Cause bodily autonomy is really what's on the ballot and that's what's on the line.
Delia Sosa: And that's the common thread between all three communities and the experiences that all of us have. All three groups just want to be able to make decisions about our own bodies and make decisions about our own lives. And if that is threatened for one group, it's going to be threatened for all of us.
That's the reality of the situation and that's what we're watching happen. We're watching it. I mean, for intersex people, bodily autonomy has been a long-standing issue and something that has never been fully available to all intersex people. But for trans people, they're trying to take away bodily autonomy. They're trying to take it away for cis women. Who are they going to come for next?
Jess Romeo: Well, I mean, this backlash has made gender affirming care so just more politicized than ever and healthcare more politicized than I think in our lifetimes. How do you stay motivated to like keep going to classes, like apply for residency, enter the field despite all of that?
Delia Sosa: Yeah, honestly, some days I'm not motivated. Some days I really just want to crawl into a hole and pretend the rest of the world doesn't exist. And when I feel like that, I have to remind myself why I went, why I wanted to do this in the first place, which was to take care of my community.
I didn't know I wanted to be an OBGYN for a while, but the common thread throughout my entire pre-med and med school experience has been that I want to care for trans and intersex people. And am in a very privileged position where I am getting an education that will allow me to do that. That is something that I don't take for granted, something that I will always be grateful for, even though I am so tired of taking exams. And I really see it as my responsibility to use the education that I have gotten and to use the position that I am in to help other people navigate the healthcare system and to make the healthcare system safer for people like us.
Jess Romeo: That's quite a responsibility.
Delia Sosa: It is. It's a responsibility, but it's also a privilege. And it's very humbling to be able to say that I'm in medical school and I'm in the process of becoming a doctor so that I can care for our communities, like specifically for that reason.
Jess Romeo: Yeah. It is pretty bad ass. Yeah, it's funny. I was just looking at one of your posts recently, and a question came up around it, like this coffee date with your younger self. I just loved it so much, but yeah.
Delia Sosa: Thank you.
Jess Romeo: Cause like, if you could sit down with your younger self, just in - and this could be a young child, this could be like middle school. What would you want them to know about who you are today?
Delia Sosa: Sorry if I get emotional about this.
Jess Romeo: I would understand completely.
Delia Sosa: I would tell them that you will survive. Some days it feels like you won't. Some days it feels like the world is caving in around you and it feels like you've fallen and can't get back up. Kind of like a life alert commercial.
But you will be able to pick yourself back up. You will keep going. You will persist. And you will be okay, even if it doesn't feel like you will be. And I would tell them that you're gonna find an incredible community, actually really multiple communities of people, who you will connect with in ways you didn't know you could connect with others. And you're going to spend the rest of your life joyfully supporting the communities that have supported you.
Jess Romeo: I'm so excited for your clinic to open. Maybe a couple more questions and then wrapping up a little bit. I'm curious. Let's see. There were a couple here that were interesting.
Delia Sosa: Yeah, sure.
Jess Romeo: Do you want to say anything more about difficulties holding the complexity of being both trans and intersex?
Delia Sosa: Yeah, yeah. I mean, for me personally, like, it just doesn't feel complex. I'm like, okay, I'm trans and I'm intersex. Like, for someone who holds those identities, it feels very simple. And I kind of have to keep reminding myself, like, for one, the majority of people are cisgender, meaning that their gender identity aligns with their designated sex at birth and their socialized gender. So it can be hard to wrap your head around what it means to be trans, first of all. And then second of all, to understand that that is different from intersex, which is having like primary and secondary sex characteristics that don't fit neatly into the male and female boxes. It's like, wait a second, doesn't that mean that you're transgender? And there's a lot of - because society has conflated gender with sex, there's a lot of confusion around what it means to be trans versus what it means to be intersex. And I have to really give people a lot of grace and a lot of patience and opportunity to grow and learn with me. I know that it's - it seems more complicated than it actually is to someone looking from the outside in.
Jess Romeo: Well, I mean, I think you started off while talking about cis folks. It's hard to understand when you never had to ask those questions for yourself. It's almost like it's a completely different language. You have to wrap your head around and then understand how to read the book. Like, you know, I can understand why it's a hard thing because I see some people conflating them. And I think, too, I'm curious for you - some intersex traits, like some androgenized traits, can feel gender-affirming. So like there - there can be some overlap. Have you had conflicting feelings about secondary sex characteristics for yourself? Has that changed over time? I could imagine it has.
Delia Sosa: It has, yeah. When I first started growing facial hair, I remember feeling so disgusted by it. I was like, "why is there hair on my face? I did not ask for this. I'm not on T. I don't understand why it's here." But the more that I've gotten to learn about not just my intersex variation and what it means for me as an intersex person, but also about my trans identity and how that manifests in my life, the more comfortable I've gotten with having facial hair and having a voice that is slightly deeper than the average female and I think honestly being intersex and finding out that I'm intersex gave me a lot more confidence and comfort in my trans identity and how that presents itself in my life and that's something that I really did not expect going into this whole intersex trans journey.
Jess Romeo: Yeah, no, I really love that because I kind of intuited that there's part of that journey there for you. And I can imagine myself, like - I don't have an intersex variation that I'm aware of, nor anything endogenously in my body helping me to live into the gender that's affirming for me. But I can imagine myself if I did kind of having that moment of being like, oh, thanks, bud. Like, you get it. You just did it.
Delia Sosa: Yeah, and like, to be honest with you, like - I logically understand that like, sex and gender are different and intersex and trans are different. But for some reason, there's something really affirming about being a non-binary person who also lives in a body that doesn't fit into a binary. Like, that feels incredible in a way that I don't even know how to explain.
Jess Romeo: Yeah. I just - not even a gender outlaw, but just the fuckery. It's great.
Delia Sosa: That's a great way to put it, yes.
Jess Romeo: It's just, yeah, it's just the fuckery. I love it. Oh, man. Well, tell me this. In the midst of like everything that's happening right now, I know it can be really difficult, but what is something that's giving you some good queer, trans, intersex, queer joy right now?
Delia Sosa: Hmm, I love this. Truthfully, being in community with other trans people has been the biggest source of joy and comfort. Like, I have been very blessed to - I hate that word blessed. I'm gonna rephrase that. I have been -
Jess Romeo: You can just, just yeah, back up. Hashtag blessed?
Delia Sosa: No.
Jess Romeo: Yeah, no, fair.
Delia Sosa: I have been very fortunate to have made a couple of wonderful friends in the intersex community and we'll just text each other a couple times a week like, what is going on in the world and can we just vent about it with each other for a few minutes? And then I also have a couple of really great trans friends who like, we all kind of take turns testifying at our respective state houses and we'll like watch each other online and record each other testifying and it's really comforting to know that like despite the world falling apart around us there are people that are in our corner and there are people who understand what it's like to live as a trans person or as an intersex person or as both.
Jess Romeo: Yeah. Yeah. We're out here. We're not going anywhere. We've always been here.
Delia Sosa: And we always will be here.
Jess Romeo: Wow, what a powerful conversation. I really enjoyed our time. Huge thanks to Delia for sharing their story and their insights. And I'm pretty sure we're going to see Delia in the future running some amazing fertility clinic for queer folks in the future. I really, I can see that so clearly.
Their dedication to building safer, more inclusive healthcare spaces is seriously inspiring and I hope this is not the end of our collaboration journey. If you want to keep up with Delia and their work, check out the links in the show notes. You can find them as @enby.delia, E-N-B-Y-D-E-L-I-A on Instagram. And please do check out information about the KIND Clinic Interact Advocates for Intersex Youth and any other links in the show notes. Thanks so much for listening. If you enjoy this episode, please don't forget to rate, share, and review. It really helps this podcast get to more people. But until next time, take care of yourselves and one another, and we'll see you here soon.
With grounded honesty and visionary clarity, Delia speaks from the heart—and from the frontlines—inviting us to imagine a healthcare system rooted in justice.
🎧 Listen now 🎧
Book Connection Corner! 📚
Looking to dive deeper into what we talked about in this episode? Check out these books from MyGenderIQ’s bookshop.org page - it vibes perfectly with our convo and adds even more insight. Plus, when you buy from our bookshop page, you’re supporting local, independent bookstores instead of megacorporations.

About your host:
Jess Romeo is a Psychiatric Nurse Practitioner, clinical social worker, mentor, and educator with a passion for making gender-affirming care more accessible, inclusive, and informed.
With years of experience seeing patients, training healthcare providers, and being queer & trans, Jess brings a nuanced, compassionate, and engaging voice to conversations about gender identity and social justice.
Through this podcast, Jess cultivates a curious and brave space to explore the realities, challenges, and triumphs of our lives—helping providers, allies, and community members reflect, deepen their knowledge, and take meaningful action.
🎙️ Be the First to Hear + Earn CEs!






